
September 2018
Advancing Primary Health Care

Pratap Patra and his wife Jyoti Rani Patri listen carefully as their Community Health Worker talks about the advantages and expected side effects of the POP- a modern contraceptive method and all the other methods of family planning available in the FP basket. Photo credit: Mubeen Siddiqui/MCSP
This October, the global community will come together in Astana, Kazakhstan for the 40th anniversary of the Alma Ata “Primary Healthcare for All” conference, and sign a new declaration committing to the advancement of primary health care in current development programs. Since that first Alma Ata conference, USAID and our partners have achieved significant advances in primary health care, enabling hundreds of millions of women, children and vulnerable populations to access preventive and life-saving health services. We believe that strong primary health care systems pave the way for countries to build healthy families, stable communities, and productive economies, which lead to self-reliance and greater security worldwide.
Our collective achievements have been just that: collaborations between governments, communities, the private sector and civil society. We believe that strengthening primary health care systems cannot be achieved by the public sector alone. There must be recognition of the potential power of communities to influence the quality of their health systems, and that private and faith-based sectors can offer more responsive care at lower or equivalent cost, of comparable or greater quality, and with better community acceptance . I have observed this first hand, after having spent a decade providing and directing pediatric primary care in underserved communities.
During October, the Agency will help build momentum for primary health care and the next global declaration by generating conversation and sharing our vision for the next 40 years and beyond. I hope you will join the conversation @usaidgh!
– Dr. Alma Golden, Senior Deputy Assistant Administrator, Bureau for Global Health
Removing Financial Hardship to Increase Access and Promote Preventive Health Services

A client presents her community-based health insurance card to a Remera-Rukoma Hospital receptionist. Photo credit: Alanna Savage/MSH.
Raissa Iradukunda and her family are covered under Rwanda’s community-based health insurance program, known locally as mutuelle de santé: “We are farmers,” she explains, “but we can afford to pay the required 3,000 Rwf (USD $3.46) per year because mutuelle de santé has enabled us to access health care even in situations where we did not have enough money for services.”
Community-based health insurance improves equity in the health system by enabling people with varying incomes to access care without fear of financial hardship. It also promotes a culture of prevention by encouraging people to use preventive health services at no additional cost. Membership premiums are income-based, meaning that enrollees pay according to their income.
After 10 years of support from USAID, the Rwanda Social Security Board now oversees ongoing management of the community-based health insurance program, with only targeted technical assistance from the Agency.
When management transitioned to the Rwanda Social Security Board, members like Ms. Iradukunda feared their families would not receive the same health benefits. However, enrollment rates actually increased after the transition, indicating the success of the Agency’s efforts to strengthen the capacity of local organizations. The Rwanda Social Security Board is managing the insurance scheme and meeting expectations of the population—a major step along the journey to self-reliance. Read more.
Village Health Workers: The First Line in Life-saving Malaria Treatment
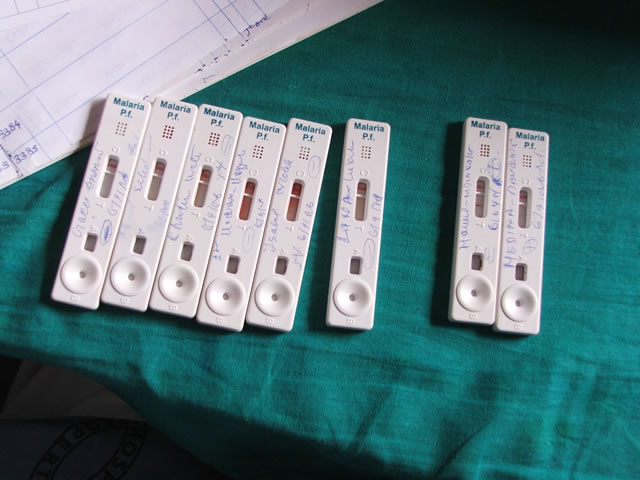 Rapid diagnostic tests (RDTs) in an Angolan clinic. Credit Angus Spiers/USAID
Rapid diagnostic tests (RDTs) in an Angolan clinic. Credit Angus Spiers/USAID
With the nearest clinic 7.5 kilometers away, the 435 households of the Zimbabwean farming community of Rujeko rely on village health workers (VHWs) for their health needs. One November night, a frantic mother showed up at VHW Mwoyounotsva Ndhlovu’s door, holding a 19-month-old baby. The boy was listless, feverish, and vomiting. Instantly, Ms. Ndhlovu recognized the signs of severe malaria, which can be deadly for children under 6.
Ms. Ndhlovu performed a rapid diagnostic test, which confirmed that the child had malaria. Pulling on latex gloves, she gave the boy 100 milligrams of rectal artesunate, a temporary treatment used in rural areas until a child can be taken to a clinic. The mother then took her son and a referral from Ms. Ndhlovu to the clinic for comprehensive care. The next day at the clinic, the child’s condition had improved and, after a few days, he was sent home to complete the course of medicine.
Ms. Ndhlovu was able to administer the life-saving artesunate because of training provided by the Zimbabwean Ministry of Health and Child Care, supported by the USAID-funded Maternal and Child Health Integrated Program and the President's Malaria Initiative.
With this training and support, VHWs can screen, diagnose and treat malaria at the community level. Malaria community case management helps ensure that communities in Zimbabwe have access to effective and life-saving malaria treatment.
USAID's Support of the Development of Malawi's National Community Health Strategy
In 2017, the Malawi Federal Ministry of Health (FMoH) launched its first National Community Health Strategy (NCHS). To guide the myriad community activities necessary for decentralization, resource constraints, increased focus on community-level prevention and promotion and quality of community health services, the FMoH needed to develop this costed actionable NCHS. The FMoH, through the Community Health Services section, led the development of the strategy with support from key partners, including the Aspen Management Partnership for Health, Dalberg Global Development Advisors, Save the Children, UNICEF, the World Bank, and USAID. Over its five- year implementation, the NCHS will contribute to reducing under-5 mortality by 25 percent and maternal mortality by 20 percent, yielding a 5-to-1 return on investment. After only one year of implementation, there has been significant progress across all strategic priorities in the NCHS. Key achievements include the dissemination of the strategy to over 1,000 district-level stakeholders, the development of a district-level implementation plan in each of the 29 districts in Malawi, the development and roll-out of three national guidelines and three training curricula for community health structures in each of the 29 districts, the appointment of a district community health coordinators for each district, and the creation of Malawi’s first Community Health Indicator Handbook, which will be the foundation of an integrated community health information system. Read more in this HuffPost article.
Engaging the Private Sector in HIV/AIDS Care: Because Comprehensive Access Requires Comprehensive Solutions

Photo credit: Martin Mugo Muiga/Horec Kenya
In Nigeria, USAID’s Sustainable Financing Initiative (SFI) for HIV/AIDS, through the U.S. President's Emergency Plan for AIDS Relief, is working with Strengthening Integrated Service Delivery for HIV/AIDS to encourage universal access to health care by increasing access to HIV services within the private sector. This helps alleviate pressure on public sector facilities and generates revenue from clients who are able and willing to pay. As a result of SFI interventions, approximately 11,995 clients now receive ARV refill services from 336 private community pharmacies.
The rapid uptake of services in this case illustrates the level of previously unmet demand for alternatives to public-sector and donor-funded services. Increasing access to HIV services by expanding services to private primary care outlets reduces stigma for HIV-positive clients, promotes self-reliance, and brings us closer to reaching sustainable epidemic control.
GLOBAL HEALTH HIGHLIGHTS

Utkrisht Bond: Improving Private Health
In September, the Utkrisht Impact Bond was featured in several publications including a report by Save the Children that released at the United Nations General Assembly. The report makes four recommendations for leveraging for global health. Forbes India and Medium also featured the Utkrisht Impact Bond’s approach and progress to date.
The Utkrisht Development Impact Bond is the first aiming to reduce maternal and newborn deaths and was developed by partners including USAID, Merck for Mothers, the UBS Optimus Foundation, PSI, Palladium and HLFPPT. Read the Save the Children report Investing in maternal and child health: Development Impact Bonds [PDF, 2.6MB], the Forbes India article Utkrisht Bond: Improving Private Health Care, and the USAID Medium article: Sharing the Responsibility.

Launch of Aspen Management Partnership for Health 2018 Impact Brief
USAID partners with Gavi, Merck for Mothers, GlaxoSmithKline, Pfizer, the UN Special Envoy for Health, and other public and private sector entities through the Aspen Management Partnership for Health (AMP Health). AMP Health partners with ministries of health to help scale community health and immunization programs by providing leadership and management training, mentoring and coaching, a network of like-minded partners, and placement of experienced private sector professionals. To date, AMP Health has catalyzed the training of 15,000 community health workers in Sierra Leone, supported the creation and dissemination of Malawi’s first-ever National Community Health Strategy and more. Read more
LOOK AHEAD
Follow @USAIDGH on on Twitter and Facebook during October as we build momentum for the second global declaration on primary health care. We’ll be sharing the hashtags, #HealthForAll and #PrimaryHealthCare with WHO and UNICEF as they run parallel primary health care campaigns. We will also be publishing a legacy report on thirty years of community based work accomplished by USAID and its partners and creating resources for partners including a social media toolkit and primary health care “playbook” which will be available online in mid-October.
G20 Health Ministerial Meeting, Argentina - October 4
Africa Health Business Symposium III - October 8–9
Africa Health Business, Johannesburg, South Africa

Fifth Global Symposium on Health Systems Research - October 8–12
Join USAID's Health Research Program on October 9 at our side session and booth at the Fifth Global Symposium on Health Systems Research, which will convene approximately 2,000 health systems researchers, policymakers and practitioners from around the world. Come learn about our research on ways to save women and children.
WHO Global Conference on Primary Health Care - October 25–26
Global Conference on Primary Health Care, Kazakhstan
USAID GH MEDIA MENTIONS
The Hidden Costs of Fistula Repair
USAID Impact Blog – September 7
The Shoulders We Stand On
IDEO.org – September 7, 2018
Partnering to Scale Impact
Duke Global Health Innovation Center – September 1, 2018
7 Transformative Digital Health Trends in International Development
ICTworks – September 19, 2018
